Coronary Microvascular Disease
What is coronary microvascular disease?
Coronary MVD affects the tiny blood vessels in the heart causing chest pain. Damage to the inner walls of these small blood vessels can cause spasms and reduced blood flow.
Women get coronary MVD more often than men, especially women with low estrogen levels, which commonly occurs in women experiencing menopause.
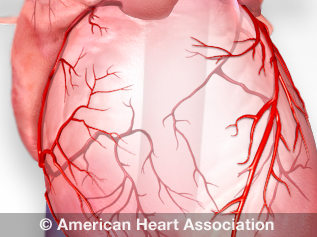
See an illustration of coronary arteries.
Other names for coronary MVD
- Cardiac syndrome X
- Nonobstructive coronary heart disease
- Small artery disease
- Small vessel disease
- Microvessel disease
What causes coronary MVD?
The same risk factors that cause plaque buildup in arteries (atherosclerosis) can also lead to coronary MVD.
Risk factors include:
- Unhealthy blood cholesterol levels
- High blood pressure
- Smoking
- Diabetes
- Overweight and obesity
- Lack of physical activity
- Unhealthy diet
- Older age, especially among women who are experiencing menopause
Understand your risk for coronary MVD
Women with low estrogen levels may be at risk for coronary MVD. Low estrogen levels before menopause can raise younger women’s risk for coronary MVD.
Women with high blood pressure before menopause are at higher risk for coronary MVD. Intense or irregular menopause symptoms can also increase the risk for heart disease. After menopause, women often have more risk factors for atherosclerosis, raising their risk for coronary MVD.
What are the signs and symptoms of coronary MVD?
Women with coronary MVD often have microvascular angina, a kind of chest pain. They might have chest pain that lasts a long time and happens at rest.
Other signs and symptoms of coronary MVD:
- Shortness of breath
- Sleep problems
- Fatigue
- Lack of energy
People with coronary MVD often first notice symptoms during daily activities and mental stress. This is different from major coronary artery disease, where symptoms usually appear during exercise. If you have coronary MVD, learn the warning signs of a heart attack and the warning signs of a heart attack in women.
Diagnosis of Coronary MVD
Your health care professional can diagnose coronary MVD based on your medical history, a physical exam and test results.
PET scans and other types of imaging can help diagnose coronary MVD. They measure blood flow through the coronary arteries and can find coronary MVD in tiny blood vessels. Cardiac catheterization and cardiac MRI with perfusion can also be used.
Diagnostic Tests
The risk factors for coronary MVD and traditional heart disease often are the same. Some tests for heart disease include:
Standard tests for heart disease may not detect coronary MVD. If you have angina but tests show your coronary arteries are normal, you could still have coronary MVD. Additional testing can confirm the diagnosis.
Coronary MVD symptoms often first happen during routine daily tasks. Because of this, you may be asked to complete the Duke Activity Status Index (DASI) questionnaire. The DASI asks questions about your ability to do daily activities.
The DASI results can help decide which additional tests are needed to diagnose coronary MVD.
Treatment of Coronary MVD
Relieving pain is one of the main goals of treating coronary MVD. Treatments can also control risk factors and other symptoms.
Treatments may include:
- Cholesterol medication to improve cholesterol levels
- Blood pressure medications to lower high blood pressure and decrease the heart's workload
- Antiplatelet medication to help prevent blood clots
- Beta blockers, calcium channel blockers or nitroglycerin to relax blood vessels
- Nitroglycerin to treat chest pain
- Surgeries such as coronary artery bypass grafting or percutaneous coronary intervention
- Enhanced external counterpulsation to apply pressure to your lower legs to improve blood flow to the heart
Prevention of Coronary MVD
You can lower your risk for heart disease by knowing your family history of heart disease and making lifestyle changes, such as:
- Managing blood pressure
- Controlling cholesterol
- Reducing blood sugar
- Getting active
- Eating better
- Losing weight
- Quitting smoking
- Getting enough sleep
- Going to cardiac rehabilitation
Your health care professional may also prescribe medications to control your risk factors. Take your medications as prescribed.